What is myasthenia gravis?
Myasthenia gravis affects how your nerves communicate with your muscles. It leads to muscle weakness that worsens throughout the day and with activity. Drooping eyelids and/or double vision are often the first sign. You may find it difficult to stand, lift objects and speak or swallow. Medications and surgery can help relieve the symptoms of this lifelong illness.
What is myasthenia gravis?
Myasthenia gravis is an autoimmune condition that causes skeletal muscle weakness. These are the muscles that connect to your bones and help you move. Myasthenia gravis usually targets the muscles in your eyes, face, neck, arms and legs. It can affect your ability to:
- Move your eyes or blink.
- Keep your eyes open.
- Make facial expressions.
- Chew, swallow and talk.
- Raise your arms up and lift objects.
- Walk upstairs or get up from a chair.
Muscle weakness gets worse after physical activity and improves after rest. Symptoms usually happen quickly.
Myasthenia gravis is a chronic (long-lasting) neuromuscular condition (it affects the junction between your nerves and muscles). There isn’t a cure, but effective treatment can help you manage your symptoms and function well.
What are the types of myasthenia gravis?
The types of myasthenia gravis include:
- Autoimmune myasthenia: It’s an autoimmune condition where the cause isn’t well understood but the likely cause is the production of certain types of antibodies (immune system proteins). This is the most common type.
- Neonatal myasthenia: A fetus gets certain antibodies from the birthing parent who has myasthenia gravis. An infant may have a weak cry or sucking reflex at birth. These temporary symptoms usually go away after three months.
- Congenital myasthenia: It isn’t an autoimmune condition, and a genetic change causes this type.
There are two subtypes of autoimmune myasthenia:
- Ocular: The muscles that move your eyes and eyelids weaken. Your eyelids may droop, or you may not be able to keep your eyes open. Some people have double vision. Eye weakness is often the first sign of myasthenia. Ocular myasthenia gravis may evolve into the generalized form for nearly half of all people diagnosed with this type.
- Generalized: Muscle weakness affects your eye muscles and others in your face, neck, arms, legs and throat. You may find it difficult to speak or swallow, lift your arms over your head, stand up from a seated position, walk long distances and climb stairs.
How common is myasthenia gravis?
Myasthenia gravis affects about 20 out of every 100,000 people around the world. The actual number may be higher, as some people with mild cases may not know they have the condition. In the United States, there are approximately 60,000 people affected by myasthenia gravis at any given time.
What are the symptoms of myasthenia gravis?
Symptoms of myasthenia gravis may include:
- Muscle weakness in your arms, hands, fingers, legs and neck.
- Fatigue.
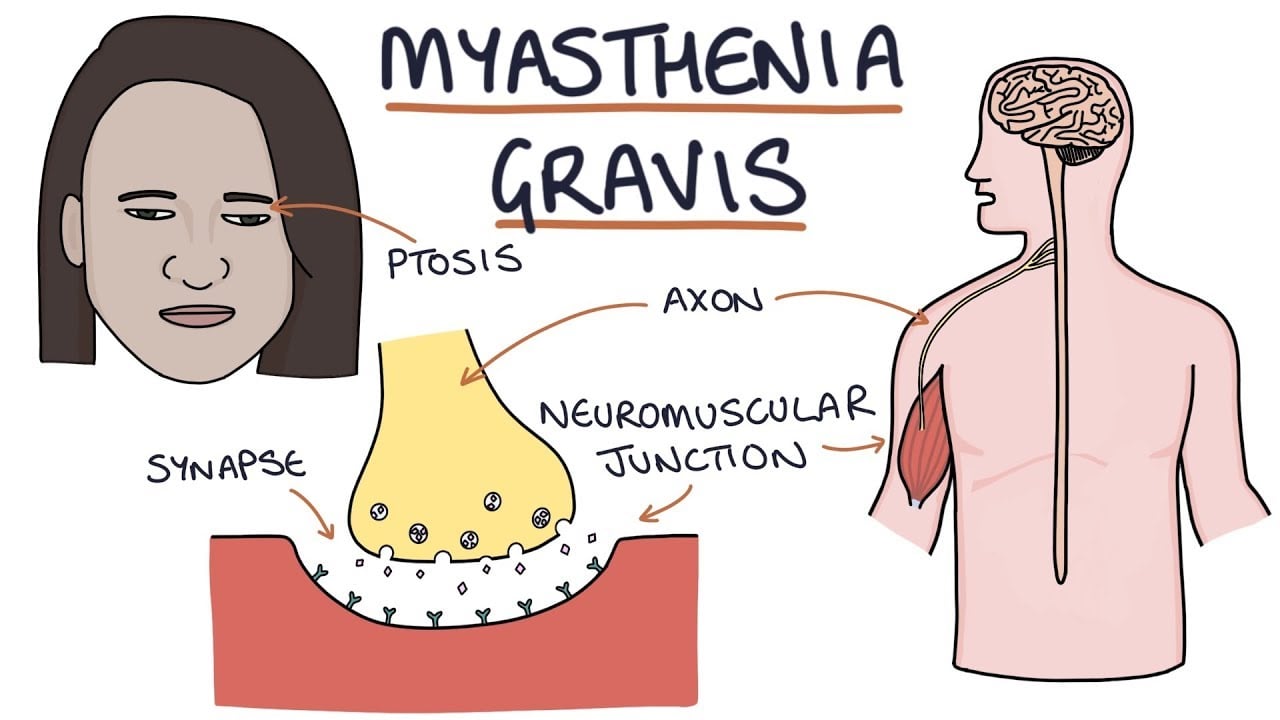
- Droopy eyelids (ptosis).
- Blurry or double vision.
- Limited facial expressions.
- Difficulty speaking, swallowing or chewing.
- Trouble walking.
Initial symptoms of myasthenia gravis happen suddenly. Your muscles usually get weaker when you’re active. Muscle strength returns when you rest. The intensity of muscle weakness often changes from day to day. Most people feel strongest at the start of the day and weakest at the end of the day.
In rare instances, myasthenia gravis affects muscles in your respiratory system. You may have shortness of breath or more serious breathing problems. Contact 911 or your local emergency services number if you have trouble breathing. In general, this doesn’t occur suddenly.
What causes myasthenia gravis?
Myasthenia gravis (autoimmune type) happens when your body’s immune system mistakenly attacks itself. Researchers aren’t sure why this happens. Studies suggest that certain immune system cells in your thymus gland have trouble identifying what’s a threat to your body (like bacteria or viruses) versus healthy components.
A genetic change causes congenital myasthenia. Antibodies passed from a birthing parent to a fetus during pregnancy cause neonatal myasthenia.
How does myasthenia gravis affect my body?
Myasthenia gravis affects communication between nerves and muscles.
When your immune system is working as expected, nerves and muscles work together. It’s similar to a baseball game:
- Nerves (the pitcher) send signals to muscles (the catcher) across a synapse (field) called the neuromuscular junction. To communicate, nerves release a molecule called acetylcholine (the baseball).
- Muscles have sites called acetylcholine receptors (the catcher’s glove). The acetylcholine binds to its receptors in the muscle tissue, like a ball landing in a glove.
- When the acetylcholine binds to its receptor, it triggers the muscle fiber to contract.
- Nerves signal muscles effortlessly, like one ball player catching a ball and throwing it to a teammate.
If you have myasthenia gravis, antibodies destroy the receptor sites, blocking nerve-muscle communication. The “catcher” can’t catch the ball, and communication becomes sluggish or doesn’t work at all.
Is myasthenia gravis inherited?
It’s rare to inherit autoimmune myasthenia gravis. You can inherit congenital myasthenia or neonatal myasthenia. Types where inheritance happens usually occur in an autosomal recessive pattern where you need two genes, one from each biological parent, to experience symptoms.
What are the risk factors for myasthenia gravis?
Myasthenia gravis is most common among women and people assigned female at birth around age 40 and men and people assigned male at birth after age 60. The condition can affect anyone at any age.
You may be more at risk of developing myasthenia gravis if you:
- Have a history of other autoimmune conditions, such as rheumatoid arthritis and lupus.
- Have thyroid disease.
If you have myasthenia gravis, your symptoms could trigger (start) if you:
- Take medications for malaria and heart arrhythmias.
- Underwent surgery.
- Had an infection.
What are the complications of myasthenia gravis?
Weakness and fatigue from myasthenia gravis can keep you from participating in activities you enjoy. This may lead to stress and depression. However, studies also show that most people with myasthenia gravis can tolerate light activities and exercises on a routine basis.
Up to 1 in 5 people with myasthenia gravis experience a myasthenic crisis or severe respiratory muscle weakness. You may need a respirator or other treatments to help you breathe. This is a life-threatening medical emergency. An estimated 20% of people with myasthenia gravis experience at least one myasthenic crisis in their lifetime.
What is the connection between the thymus gland and myasthenia gravis?
Many people with myasthenia gravis have thymus gland conditions that may trigger symptoms. The thymus is a small organ in your upper chest. It’s part of your lymphatic system. It makes white blood cells that fight infections. Two-thirds of people with myasthenia gravis have overactive thymic cells (thymic hyperplasia). About 1 in 10 people with myasthenia gravis have thymus gland tumors called thymomas, which may be benign (not cancer) or cancerous.
Diagnosis and Tests
How is myasthenia gravis diagnosed?
To diagnose myasthenia gravis, your healthcare provider will perform a physical exam and ask detailed questions to learn more about your symptoms and medical history. Testing confirms a diagnosis. It may include:
- Blood antibody tests: About 85% of people with myasthenia gravis have unusually high levels of acetylcholine receptor antibodies in their blood. Approximately 6% of people diagnosed have muscle-specific kinase (MuSK) antibodies.
- Imaging scans: An MRI or CT scan can check for thymus gland problems like tumors.
- Electromyography (EMG): An EMG measures the electrical activity of muscles and nerves. This test detects communication problems between nerves and muscles.
Myasthenia gravis stages
There are five main classifications of myasthenia gravis that your healthcare provider may use during a diagnosis:
- Class I: Muscle weakness only affects your eyes (ocular muscle).
- Class II: Muscle weakness is mild.
- Class III: Muscle weakness is moderate.
- Class IV: Muscle weakness is severe.
- Class V: Severe muscle weakness affects how you breathe. You may need intubation or mechanical ventilation.
Management and Treatment
How is myasthenia gravis treated?
There’s no cure for myasthenia gravis. But effective treatment is available to help manage your symptoms. Treatments may include:
- Medications: Certain medications can reduce your symptoms.
- Monoclonal antibodies: You’ll receive intravenous (IV) or subcutaneous (SQ) infusions of biologically engineered proteins. These proteins suppress an overactive immune system.
- Plasma exchange (plasmapheresis): An IV connected to a machine removes harmful antibodies from your blood plasma and replaces them with donor plasma or a plasma solution.
- IV or SQ immunoglobulin (IVIG or SCIG): You’ll receive IV infusions of donor antibodies over two to five days. IVIG or SCIG can treat myasthenia crisis, as well as generalized myasthenia gravis.
- Surgery: A thymectomy is surgery to remove the thymus gland.
Myasthenia gravis medications
Common medications to treat myasthenia gravis include:
- Cholinesterase inhibitors (anticholinesterase): They boost signals between nerves and muscles to improve muscle strength.
- Immunosuppressants: Medications like corticosteroids decrease inflammation and reduce your body’s production of abnormal antibodies.
Side effects are possible with these medications. Talk to your healthcare provider to learn more before starting a new medication.
How can I alleviate myasthenia gravis symptoms?
If you have myasthenia gravis, try these steps to ease fatigue and boost muscle strength:
- Exercise regularly to strengthen muscles, boost your mood and give you more energy. Talk to your healthcare provider before starting an exercise program to make sure it’s safe.
- Avoid going outside in the middle of a hot day. Apply cold compresses to your neck and forehead when you feel overheated. Heat can make your symptoms worse.
- Get plenty of protein and carbohydrates in your meals for added energy.
- Tackle your most exhausting tasks earlier in the day when you feel your best.
- Take naps or rest breaks throughout the day.
Outlook / Prognosis
What’s the outlook for myasthenia gravis?
Myasthenia gravis is a treatable condition. Symptoms range from mild to severe. Symptoms tend to reach their peak in severity within one to three years of initial diagnosis.
Most people with the condition live full and active lives with treatment.
Some cases go into remission. Remission is when your symptoms stop for a period of time. This could be temporary or permanent. If remission happens, your healthcare provider may adjust your treatment plan.
What is the life expectancy of a person with myasthenia gravis?
Most people have a normal life expectancy with myasthenia gravis. Life-threatening outcomes may happen during a myasthenic crisis, which affects your ability to breathe.
How does myasthenia gravis affect pregnancy?
In rare instances, pregnancy brings on myasthenia gravis symptoms for the first time. If you already have this condition, symptoms may worsen during the first trimester or immediately after childbirth. In some cases, myasthenia gravis symptoms improve during pregnancy.
Certain treatments aren’t safe during pregnancy or breastfeeding (chestfeeding). Your healthcare provider can guide you through this time, ensuring a healthy pregnancy.
Living With
When should I see a healthcare provider?
You should call your healthcare provider if you experience:
- Blurred or double vision.
- Difficulty walking, talking or eating.
- Extreme muscle fatigue or weakness.
- Shortness of breath.
Call 911 or your local emergency services number if you have trouble breathing.
What questions should I ask my healthcare provider?
You may want to ask your healthcare provider:
- What caused these symptoms?
- What’s the best treatment option for me?
- What are the treatment side effects?
- What lifestyle changes should I make?
- Should I look out for signs of complications?
- Can I start an exercise program safely?
- Is there a patient support group I can join?
- Is there a research project I can participate?
A note from Cleveland Clinic
It’s challenging to live with a chronic illness like myasthenia gravis. When you want to be active, you might feel too tired or weak to participate. This can take a toll on your mental and physical health over time. Although there isn’t a cure, most people with this condition lead full and active lives with treatment. Severe disabilities from myasthenia gravis are extremely rare. Your healthcare provider can suggest ways to manage symptoms so you can feel better.